Recently, our small community received the news of three new families now living with T1D. As always (now through a cure) my heart not only breaks but I also feel this long inspired determination to help each newcomer adapt and adjust to the best life with T1D possible. Because I am on a kick with Twitter hashtags @natsweetsisters, these are a few of my favorites:
#togetherwecan #improveT1D
They kind of ring a perfect bell, right? The girls and I think so too!
Along with that, I have spent over a decade testing the analogy that within T1D, kids are first and diabetes is second. Always. I firmly believe that we can live our lives in the fullest manner possible if we remind ourselves of that cherished motto. There are no limitations when you decide how best to fit T1D INTO YOUR LIFE and not, fitting your life into T1D. Wash and repeat. It's a powerful, cleansing mantra!
And it works well, especially during the Halloween holiday madness.
To begin with, just ask yourself a few questions.
1.) What was Halloween like before T1D?
2.) What would you like Halloween to be like after T1D?
My guess is that most of us, would enjoy a carefree Halloween just as it was before T1D. The great news is that is VERY doable!
The lesson that I learned regarding food and holidays, is that to children, it is NOT about the candy. It is about the gathering, counting, bragging and admiring of the candy. On Halloween, kids are working to amass as much candy as quickly as possible. If you have ever observed the evening shenanigans, you might have noticed costumed children literally running from door to door. The little (and big) kids barely slow down in their efforts to ring as many doorbells as possible. It is one of the reasons that masks are not as favored; the kiddos need to see to be able to run while avoiding sprinklers, lawn art and benches. The same spirit of excitement holds true at fun Halloween style carnivals and Trunk-or-Treat events. Kids run and parents yell, "Slowwwwww down!". I don't know about you, but mysteriously, on Halloween, my kids could never hear me.
Once the speed candy gathering has ended, there is often a need for some of that beloved candy. Blood sugars that spiked in excitement, start to regress and drop as blood sugar moves down. A well timed sugary treat is often wonderful and as parents, the value of the gathered candy increases. Suddenly, the candy isn't as much of a nuisance as it is a refreshingly 'free' replenishment of low blood sugar goodies. Thank you to our friends and neighbors for helping out!
As you wind your way back home, the tabulating and bragging begins. Many kids do not want to even eat the candy at the start as it will take their stash of 45 snickers and 26 kit kats down by one. After a round of selfie candy pictures, the kids like the idea of knowing that it is their candy and will place it into a special plastic container marked with their name and attempt to hide it within the family pantry.
You may notice the volume increase within your house. Giggly stories may be shared about the family that gave handfuls of full size candy-bars or about the one odd house that passed out coupons. Soon after, quiet resumes and bedtime will ensue and then, Halloween will be another happy memory just as it was before T1D.
Here are a few fun ways to continue to enjoy Halloween:
1.) Print up
Halloween Carb Candy Counts and bring them along as you Trick-Or-Treat. I also like to tape a set onto the plastic container or bag that will hold the candy within the pantry before we return home. That way, everything is ready to be stored and if someone wants to eat it without me, I have a much higher chance of seeing an appropriate bolus.
2.) If some of the candy is not suitable, make sure you clearly discuss the reasons with your child (Chewy candy for braces, nut candy for allergies, scary weird serial killer candy that should be thrown out). Try not to say
"because of T1D". After all, we know that all of our kids can eat a healthy, balanced variety of foods, which for kids includes the occasional sweet treat.
3.) If a Halloween Witch came to take the candy BEFORE T1D, then a Halloween Witch may want to come after T1D. The best way to make a relaxed and fun evening is to follow the pattern that you had prior to diagnosis.
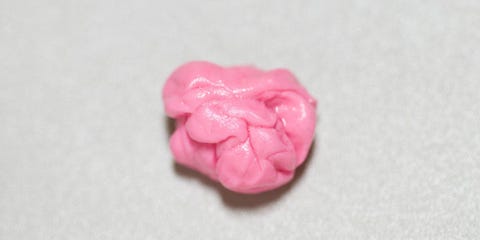
4.) Serve a well planned meal before heading out. Running around the neighborhood takes a lot of energy. As part of the festivities, our family likes to enjoy a fun meal of mummy hot dogs, ghost cheese shapes and crackers, veggie monsters
(use toothpicks to create fun characters with broccoli, olives, carrots and celery. Cream cheese makes great eyeballs) and lots of ghoulish water - black water
(our Kroger store carries this) is a fun treat for setting the theme of the evening.
As a bonus idea, if your loved one with T1D is using multiple injection therapy, having food available for a meal after the trick-or-treating is a wonderful way to blend the carbs of candy into the carbs of dinner. No extra injection needed. Going forward after Halloween, it is easy to add a few treats to each mealtime bolus injection to avoid extra shots too.
5.) Have friends join in the fun. This is a neat way to help show the world that T1D is limitless, even on Halloween. Your loved one with T1D can do anything that they want! Including enjoying a caramel apple or a butterfinger. Or three.
Happy Halloween!
From the Naturally Sweet Sisters